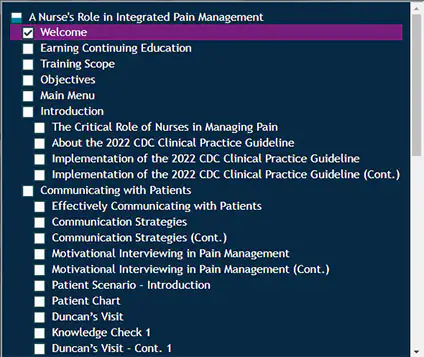
2022 CDC Clinical Practice Guideline
CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022
CDC's 2022 Clinical Practice Guideline for Prescribing Opioids for Pain training module (CDC)
Opioid Overdose Prevention Resources for Health Care Providers (CDC)
Clinical Practice Guideline at a Glance (CDC)
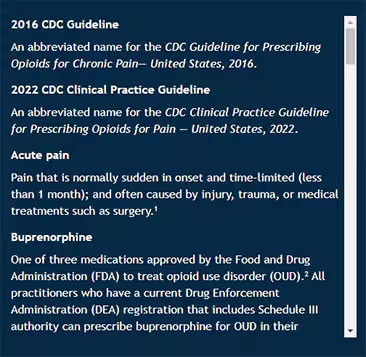
Health Equity
The Future of Nursing 2020-2030 Charting a Path to Achieve Health Equity (National Academies)
Office of National Drug Control Policy Changing the Language of Addiction (PDF)
(PDF)
Words Matter - Terms to Use and Avoid When Talking About Addiction (NIDA)
Language, Substance Use Disorders, and Policy: The Need to Reach Consensus on an "Addiction-ary"
Breaking Through the Wall of Stigma (NIH)
Naloxone
Naloxone training modules (CDC)
Naloxone conversation starters (CDC)
Nonopioid Therapies
Nonopioid Therapies for Pain Management (CDC)
Opioid Use Disorder
Addiction Medicine Toolkit (CDC)
Assessing and Addressing Opioid Use Disorder (OUD) training module (CDC)
Linking People with Opioid Use Disorder to Medication Treatment (CDC)
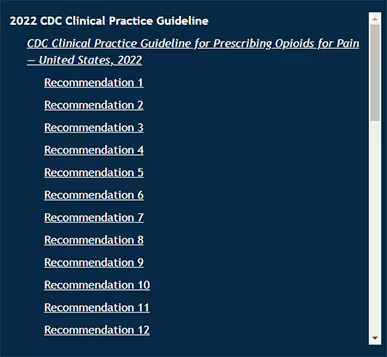
2016 CDC Guideline
An abbreviated name for the CDC Guideline for Prescribing Opioids for Chronic Pain— United States, 2016.
2022 CDC Clinical Practice Guideline
An abbreviated name for the CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022.
Acute pain
Pain that is normally sudden in onset and time-limited (less than 1 month) and often caused by injury, trauma, or medical treatments such as surgery.1
Buprenorphine
One of three medications approved by the Food and Drug Administration (FDA) to treat opioid use disorder (OUD).2 All practitioners who have a current Drug Enforcement Administration (DEA) registration that includes Schedule III authority can prescribe buprenorphine for OUD in their practice if permitted by applicable state law.
Care coordination
Deliberate organization of patient care activities and information sharing among all participants involved in a patient's care, such as clinicians, caregivers, and/or social workers, to achieve safer and more effective care.3
Chronic pain
Pain that typically lasts longer than three months. Chronic pain can be the result of an underlying medical disease or condition, injury, medical treatment, inflammation, or unknown cause.1
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)
A classification of mental disorders with associated criteria designed to facilitate more reliable diagnoses of these disorders.4
Implicit bias
An unconscious or automatic mental association made between members of a group and an attribute or evaluation.5
Medications for opioid use disorder (MOUD)
Three Food and Drug Administration (FDA)-approved medications to treat opioid use disorder (OUD): methadone, naltrexone, and buprenorphine.6
Methadone
One of three medications approved by the Food and Drug Administration (FDA) to treat opioid use disorder (OUD). It can only be prescribed or dispensed for OUD through a Substance Abuse and Mental Health Services Administration (SAMHSA) certified Opioid Treatment Program (OTP) for daily administration either on site or, for certain patients, at home.
Microaggressions
Brief and commonplace daily verbal, behavioral, or environmental indignities, whether intentional or unintentional, that communicate hostile, derogatory, or negative racial slights and insults toward people of color.5
Motivational Interviewing
A collaborative conversation style for strengthening a person's own motivation and commitment to change.7 MI is patient-centered, collaborative, and guiding. It enhances a patient's intrinsic motivation to change behavior and helps patients explore and resolve contradicting feelings or ideas.
Naloxone
A lifesaving drug, recognized by common brand names like Narcan, that can reverse the effects of opioid overdose if administered in time.
Naltrexone
One of three medications approved by the Food and Drug Administration (FDA) to treat opioid use disorder (OUD). Naltrexone is not a controlled substance, so it may be prescribed or dispensed by any clinician who is licensed to prescribe medications.
Nonopioid pharmacologic therapies
Non-opioid medications for pain, including acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), selected anticonvulsants, and selected antidepressants, among others.
Nonopioid therapy
Methods of managing pain that do not involve opioids. This can refer to both pharmacologic therapies (medication) and nonpharmacologic therapies. These methods can include, but are not limited to, non-opioid medications, cognitive behavioral therapy, physical therapy, acupuncture, meditation, exercise, or interventional therapies like injections.8
Nonpharmacologic therapies
Treatments that do not involve medications, including, but not limited to, physical treatments (e.g., exercise therapy, massage) and behavioral treatments (e.g., cognitive behavioral therapy, mindfulness-based stress reduction).
Opioid use disorder (OUD)
A problematic pattern of opioid use leading to clinically significant impairment or distress. A diagnosis of OUD is based on specific Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, including but not limited to unsuccessful efforts to cut down or control use, or use resulting in social problems and a failure to fulfill obligations at work, school, or home.4
Social determinants of health (SDOH)
Nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.9
Subacute pain
Pain with a duration of at least one month and up to three months.1
Stigma
Discrimination against an identifiable group of people. For people with substance use disorders (SUDs), stigma may stem from beliefs that people with SUDs are at fault for their disease and are incapable of being treated.10 People with SUDs may internalize this stigma leading to a reluctance to seek help.
1 Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. (2022). MMWR Recommendations and Reports; 71(No. RR-3):1–95. DOI: http://dx.doi.org/10.15585/mmwr.rr7103a1
2 Substance Abuse and Mental Health Services Administration (SAMHSA). (2022, March). Buprenorphine. Retrieved from https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenorphine
3 Agency for Healthcare Research and Quality. (2018, August). Care Coordination. Retrieved September 6, 2022, from https://www.ahrq.gov/ncepcr/care/coordination.html
4 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013.
5 National Academies of Sciences, Engineering, and Medicine. 2021. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington, DC: The National Academies Press. https://doi.org/10.17226/25982 .
.
6 Treatment Improvement Protocol (TIP) Series 63: Medications for Opioid Use Disorder. (2021). Substance Abuse and Mental Health Services Administration. Publication No. PEP21-02-01-002. Retrieved September 6, 2022, from https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-02-01-002.pdf
7 Miller, W. R., and Rollnick, S. (2013). Motivational interviewing: Helping People Change. (3rd ed.) New York: Guilford Press
8 Centers for Disease Control and Prevention (CDC). (2021, Jan). Commonly Used Terms. Retrieved from https://www.cdc.gov/overdose-prevention/glossary/index.html
9 Centers for Disease Control and Prevention (CDC). (2022, Dec). Social Determinants of Health at CDC. Retrieved from https://www.cdc.gov/about/sdoh/index.html
10 National Institute on Drug Abuse. (2021, May 25). Words Matter – Terms to Use and Avoid When Talking About Addiction. Retrieved May 27, 2021, from https://www.drugabuse.gov/nidamed-medical-health-professionals/health-professions-education/words-matter-terms-to-use-avoid-when-talking-about-addiction